Rotator Cuff Injury: Understanding the Recovery Timeline and Surgical Care
If you’ve been diagnosed with a rotator cuff injury, one of your first concerns is understandably: “How long will it take to heal?” The duration of recovery varies significantly based on the severity of the tear, the nature of the treatment (conservative vs. surgical), and individual patient factors such as age, health status, and adherence to rehabilitation.
This comprehensive guide outlines the anatomical basis of the rotator cuff, classifications of injury, treatment modalities—including surgical intervention—and realistic recovery expectations to empower you throughout your healing journey.
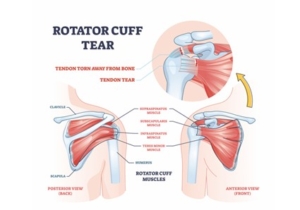
What Is the Rotator Cuff?
The rotator cuff is a functional group of four muscles and their associated tendons that stabilise the glenohumeral (shoulder) joint and facilitate essential arm movements. These muscles include:
- Supraspinatus – Initiates shoulder abduction
- Infraspinatus – External rotation
- Teres Minor – Assists with external rotation
- Subscapularis – Responsible for internal rotation
Injury to any of these components can compromise shoulder function, resulting in pain, weakness, limited mobility, and disrupted biomechanics. These injuries may result from acute trauma (e.g., falls) or chronic degenerative processes.
Diagnosis typically involves clinical examination and confirmation via imaging modalities such as MRI or ultrasound to determine the extent of tendon pathology.
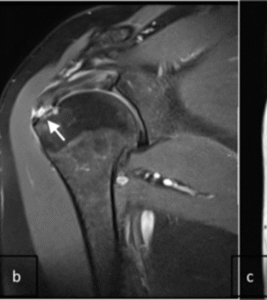
MRI image demonstrating rotator cuff tear
Types of Rotator Cuff Injuries
Rotator cuff injuries can range in severity and are classified as follows:
- Tendinitis or Bursitis: Inflammation caused by overuse, repetitive motion, or impingement
- Partial Thickness Tear: The tendon is damaged but not fully detached from the humeral head
- Full-Thickness Tear: The tendon is completely torn away from the bone, often requiring surgical repair
What Does Rotator Cuff Surgery Involve?
Surgical intervention is commonly indicated in the presence of full-thickness tears, persistent pain, or functional impairment despite conservative management.
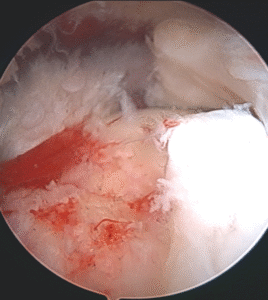
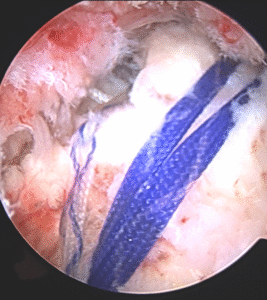
- Arthroscopic Repair: The preferred technique involving small incisions and a fibre-optic camera (arthroscope). Sutures and bioabsorbable anchors reattach the tendon to the humeral head. Full description of technique is in the link below https://youtu.be/3OaWXXEdS7g
- Open or Mini-Open Repair: Reserved for complex or massive tears not amenable to arthroscopy
- Additional Procedures: Subacromial decompression, acromioplasty, or bursal excision may be performed concurrently to address impingement or inflammation
Post-surgical success depends heavily on anatomical tendon reattachment and structured postoperative rehabilitation.
Arthroscopic images showing rotator cuff tear and repair.
Risks and Complications of Rotator Cuff Surgery
While generally safe, rotator cuff repair surgery is not without risks. Potential complications include:
- Infection – Rare and usually managed with antibiotics
- Nerve Injury – Uncommon but possible due to surgical proximity
- Stiffness and Frozen Shoulder (Adhesive Capsulitis) – Preventable with early mobilisation under guidance
- Re-Tear – More likely in larger tears or patients with poor tendon quality
- Complex Regional Pain Syndrome (CRPS) – Rare but serious, characterised by prolonged pain
- Deep Vein Thrombosis (DVT) – Preventable with mobility and thromboprophylaxis
Meticulous surgical technique, preoperative assessment, and postoperative monitoring are essential to mitigate these risks.
Anaesthetic Considerations
- General Anaesthesia – Ensures unconsciousness during the procedure
- Interscalene Nerve Block – A regional block that provides extended postoperative pain relief and reduces the need for opioids
- Sedation with Regional Anaesthesia – May be considered for suitable candidates based on anaesthetic evaluation
Postoperative Immobilisation: Sling Use
A shoulder sling is typically required for 4 to 6 weeks postoperatively to allow adequate tendon healing and minimise strain on the repair. Duration may vary depending on:
- The size and complexity of the tear
- Integrity of the repair
- Surgeon’s intraoperative assessment
During this period, gentle pendulum exercises may be introduced to prevent stiffness without compromising the repair.
Postoperative Pain Management
Pain control is managed through a multimodal strategy, including:
- Interscalene block for immediate relief
- Oral analgesics such as acetaminophen, NSAIDs, and short-course opioids
- Cryotherapy (ice packs) to reduce swelling and discomfort
An effective pain management plan is key to early mobilisation and optimal physiotherapy participation.
Daily Activities and Lifestyle Adjustments
During the initial recovery phase, patients often require assistance with:
- Dressing, grooming, and household chores
- Modifying home environments (e.g., using slip-on clothing, front-fastening garments)
- Sleeping in a reclined position with arm support to alleviate discomfort
Occupational therapy may be recommended to facilitate safe return to functional independence.
Initiating Physiotherapy: When and How Often?
- Passive exercises typically begin between 2 to 4 weeks post-op, supervised by a physiotherapist
- Active range-of-motion (ROM) exercises are introduced around 6 weeks
- Strengthening commences at 3–4 months, depending on healing and progress
Physiotherapy sessions may occur once or twice weekly, with daily home exercises being essential to recovery.
Postoperative Wound Care
- Maintain a clean, dry surgical site to prevent infection
- Follow your surgeon’s dressing change instructions
- Do not forcibly remove steri-strips—they will naturally detach within 10–14 days
- Avoid submersion in water until cleared for full healing
- Watch for signs of infection: redness, warmth, drainage, or fever
Healing Timeline: How Long Does It Take?
| Injury Type | Estimated Recovery Time |
|---|---|
| Tendinitis/Bursitis | 2 to 6 weeks |
| Partial-Thickness Tear | 2 to 3 months (non-surgical) |
| Full-Thickness Tear (Surgical) | 4 to 6 months or longer |
Several factors including age, health status, surgical complexity, and adherence to physiotherapy play a critical role in healing duration and functional outcomes.
Final Thoughts
Although rotator cuff injuries can be debilitating, most patients regain near-complete shoulder function with timely intervention, structured rehabilitation, and a proactive recovery mindset. Early diagnosis and patient education are essential to minimising complications and optimising long-term results.
If you are uncertain about your progress or experiencing ongoing symptoms, consult a shoulder specialist or orthopaedic surgeon for individualised assessment and guidance.

Leave a Reply
Want to join the discussion?Feel free to contribute!